Sleep Apnea
In Bergen County, New Jersey & NYC
As a leading sleep apnea expert, Dr. Monica Tadros offers a wide range of sleep disorder treatments using the latest airway pressure (PAP) devices, oral appliances, and surgical methods.
What Is Obstructive Sleep Apnea?
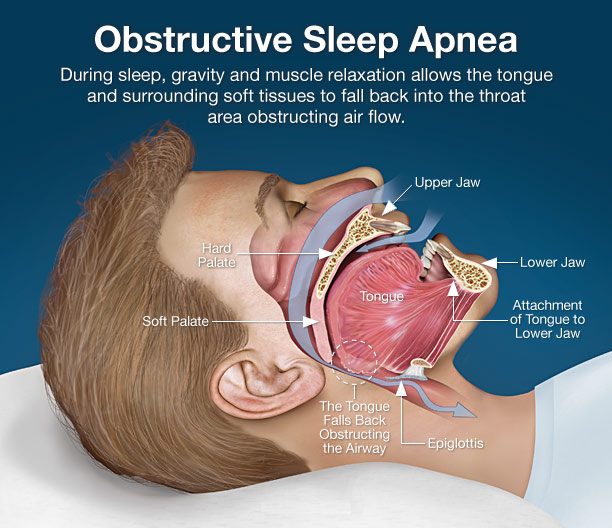
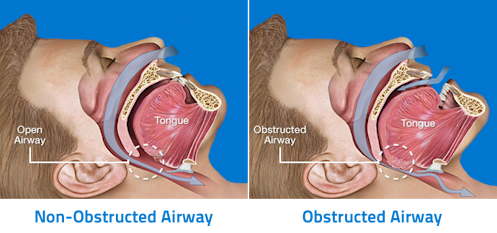
Obstructive Sleep Apnea (OSA) is a disorder in which normal breathing is interrupted during sleep due to the blockage of airflow in the upper airway breathing passages. Most commonly, sleep apnoea occurs when the muscles in the back of the throat relax as we enter our more restful deep stages of sleep (Stage 3) or our dream state (REM) sleep. Episodes of sleep apnea may occur hundred of times every night and are linked to changes in heart rate, loud breathing sound, and a decrease in oxygen saturation.
Dr. Monica Tadros offers the most advanced upper airway surgery options to reduce the degree of obstruction in the nose. Depending on the severity of Obstructive Sleep Apnea (OSA), Dr. Tadros may utilize nasal surgeries, palatal surgeries, and tongue-based surgeries to alleviate and treat OSA.
While being the most trusted and respected plastic surgeon in NJ and NYC, Dr. Tadros utilizes her innovative approach to treating OSA. Her enormous experience, coupled with attention to detail, has earned Dr. Tadros one of the most respected reputations in New Jersey.
Dr. Monica Tadros of the center for snoring surgery specializes in sleep apnea treatments in Englewood, NJ & NYC. Obstructive Sleep Apnoea affects approximately 18 million adults in the United States.
Dr. Tadros accepts most POS and PPO insurances for any medical issues related to the nose as an out-of-network provider. Please contact us today or call New York City: (201) 408-5430 or New Jersey: (201) 408-5430.
Sleep Apnea In-Depth
Blockage of airflow during sleep apnea causes prolonged hypoxia (low levels of oxygen) in the blood. As the concentration of carbon dioxide builds up in the bloodstream, the brain finally overrides the lapse in breathing, forcing the patient into a lighter stage of sleep (stage 1 or 2) to reposition and resume breathing. Since obstructive occurs in the deep stages of sleep, it is unrecognized by the individual who never fully wakes up.
Extreme fatigue and unrestful sleep result from sleep apnea because the patient fails to enter the restorative stage 3 deep sleep. A sleep study called a polysomnogram is important to evaluate all sleep-disordered breathing.
Positional statistics can help differentiate different areas of obstruction and causes of sleep disorder. This testing will also help differentiate OSA from the less common neurologic condition called central sleep apnoea, in which the brain fails to initiate or control breathing during sleep.
Dr. Monica Tadros is a best-rated expert in treating sleep apnea. She can restore your sleep and correct sleep disorders in our office located in Englewood, Bergen County, New Jersey.
How Is Obstructive Sleep Apnea Treated?
Many factors contribute to OSA, and a thorough evaluation by your local doctor Dr. Tadros requires a sleep disorder study and comprehensive airway examination that highlights: nasal obstruction (deviated nasal septum/turbinate overgrowth), tonsil enlargement, soft palate laxity, and uvula enlargement oropharyngeal tissue hypertrophy (overgrowth) tongue enlargement (macroglossia) and hyoid bone position epiglottis position.
Primary treatment includes a trial of CPAP (continuous positive airway pressure) appliance during sleep and goal-directed weight loss. Adjunct sleep apnea-related procedures may include an oral dental appliance or nasal surgery to decrease airway pressures and improve CPAP comfort and compliance.
Some patients cannot tolerate or comply with CPAP and should be evaluated by a sleep apnea specialist. Depending on the severity of sleep disorders and the associated pathology, a number of procedures may open the airway, improve snoring, and diminish apneic events. A variety of sleep apnoea procedures can be used to tailor a sleeping disorder treatment regimen.
Image Source: Dear Doctor, Inc.
Why Is the Treatment of Obstructive Sleep Apnea (OSA) Important?
OSA causes persistently low levels of oxygen in the blood for a significant portion of the night. This sleep apnoea forces the body to work hard to pump blood in order to oxygenate the brain and organ and leads to one of the most unrecognized causes of silent hypertension.
Over many years, the sleep disorder can lead to uncontrolled weight gain, heart disease, gastroesophageal reflux disease (GERD), diabetes, and depression. Am I a candidate for a Sleep Apnea Evaluation? Schedule your consultation today.
Medical Conditions Associated with Sleep Apnea
When your sleep is disturbed by Snoring and Sleep Apnea, many problems can occur. Decreased blood flow to the brain and body can lead to:
- Heart Attack;
- Heart Disease;
- Stroke;
- Diabetes;
- High Blood Pressure;
- Sexual Dysfunction;
- Memory Loss;
- Daytime Sleepiness;
- Depression;
- Lower Cognitive Ability;
- Obesity;
- Carotid Artery problems
Nonsurgical Treatments for Sleep Apnea
The most widely used and effective sleep apnea procedure is continuous positive airway pressure (CPAP). A CPAP machine has a mask that you wear at night that gently blows air into your airways to keep them open while you sleep. However, you should be aware that CPAP machines have been criticized for being uncomfortably big and noisy, preventing many patients from getting proper sleep and achieving long-term compliance.
Some patients with mild to moderate OSA prefer an oral appliance because it is small, portable, and easy to use. The custom-fitted oral appliance helps hold the tongue or support the jaw in a forward position while you sleep, reducing airway collapsibility. An oral appliance is typically used when patients are unable to tolerate CPAP therapy, but it can also be combined with a CPAP machine for achieving the best results in treating stubborn cases of sleep apnea.
Surgical airway correction may be an option if you cannot tolerate other treatment methods or remain symptomatic despite their use.
Determining If Surgery Is Right for You
Individuals who have tried CPAP for several weeks and were unable to tolerate it are usually candidates for sleep apnea surgery. In adult patients, surgery is rarely indicated as a first-line treatment. In children, however, adenotonsillectomy is commonly recommended as first-line therapy for moderate-to-severe cases accompanied by adenotonsillar hypertrophy. When determining whether the surgery is right for you, Dr. Tadros, one of the best sleep disorder doctors in NYC and NJ, will carefully consider the following indications for surgical airway correction of OSA:
- Innaficcinecy of other treatment methods or non-compliance with noninvasive forms of treatment
- An increased respiratory disturbance index (RDI) with significant daytime somnolence (EDS)
- Oxygen desaturations below 90%
- Medical comorbidities such as hypertension and arrhythmias
- Anatomic abnormalities of the upper airway
What Are the Contraindications to OSA Surgery?
Contraindications for OSA surgery vary depending on the procedure. However, here are a few general examples:
- A problem that surgery can’t treat
- Poor emotional and physical health
- Unrealistic expectations of the outcomes
- An active infection
- Bleeding or clotting disorders
In addition, medical conditions that make the use of general anesthesia impossible are also a relative contraindication to surgery for OSA.
Surgery for Obstructive Sleep Apnea
Sleep apnea surgery is a multi-step process that normally requires more than one procedure. The surgical procedures must be chosen based on your unique anatomy and sleep study findings and are carried out in stages depending on your obstruction site.
The fundamental goal of your sleep apnea surgery specialist is to improve or eliminate sleep-associated airway collapse while maintaining normal upper airway and related functions such as speech and swallowing. Surgical sleep apnea treatment can consist of either soft tissue removal or skeletal modification. The most commonly used procedures for OSA include:
- Uvulopalatopharyngoplasty (UPPP) aims at removing the excess tissue from the soft palate and the back of your throat in order to widen the airway and allow air to travel more easily through the throat when you breathe.UPPP is not endorsed as a sole procedure for treating OSA. According to an article published on NCBI, the reported success rate of UPPP as a treatment for OSA ranges between 16% and 83%, depending on how a positive outcome is defined. Post-operative risks associated with UPPP include elopharyngeal insufficiency, dysphagia, and nasopharyngeal stenosis. The surgery is performed in the operating room under general endotracheal anesthesia. Full recovery takes 2 to 3 weeks.
- Hyoid myotomy and suspension aims at increasing the size and improving the stability of the airway behind and below the base of the tongue by pulling forward the hyoid bone and the muscles that attach it to the tongue.Hyoid myotomy and suspension surgery is often done in conjunction with other procedures. When paired with genioglossus advancement and UPPP, this procedure shows a 61% success rate. The procedure can be done with a little incision and a minimally invasive approach, resulting in lower risks of complications and reduced patient morbidity. This procedure is performed in the operating room under local anesthesia, and you can expect to recover fully within 2 to 3 weeks.
- Advancement genioplasty entails cutting the patient's own chin bone and moving it forward, allowing the patient to breathe more easily throughout the night.The procedure's success rate varies, ranging from 23% to 77%. As a result, it's usually combined with UPPP to achieve the best outcomes. Infection, haematoma, damage to the genioglossus muscle, and paraesthesia of the lower teeth are all risks associated with the surgery. The procedure is performed as an inpatient in a hospital under a general anesthetic. Recovery can take up to 4 weeks.
- Maxillo-mandibular advancement aims at moving the upper and lower jaw forward to enlarge the airway in both the palate and tongue regions. This procedure may be necessary to perform together with advancement genioplasty in severe cases of obstructive sleep apnea-hypopnea syndrome.Although this procedure’s success rate is relatively high (87%), it should be performed only in severe cases due to the risk of significant changes in the patient’s physical appearance. This procedure is carried out in a surgical center or operating room under general anesthesia. The recovery is slow and typically takes 2 to 3 months.
- Tonsillectomy entails removing swollen tonsils and adenoids that block your airway in order to improve your breathing.Tonsillectomy is regarded to be safe and effective in children over the age of two, with cure rates ranging from 60% to 80%. It can also be used in adult patients with tonsillar hypertrophy. Local anesthesia in conjunction with general will be provided to keep you safe and comfortable during the procedure. You will be discharged from the surgical center on the day of surgery. Recovery time is usually 1 to 2 weeks.
- Tracheostomy is the last resort option that involves creating an opening through the front of the neck and into the cervical trachea. This allows oxygen to be delivered to the lungs while completely bypassing the closed upper airway.Tracheostomy is usually recommended for people who have significant obesity, concurrent obesity hypoventilation syndrome, or severe craniofacial deformities. Despite the fact that this procedure is invasive and disfiguring and may have a psychosocial impact on the patient's life, it considerably reduces AHI while consistently increasing ESS scores, resulting in lower mortality compared to untreated OSA patients. Tracheostomy is performed in an operating theatre under general anesthesia. Regional anesthesia may be chosen to avoid perioperative respiratory complications in obese OSA patients. It will take a couple of days for you to get used to breathing through a tracheostomy tube and a few weeks to fully adjust to living with it.
- Hypoglossal nerve stimulation involves implanting a stimulating device into the chest to sense diaphragmatic contraction and activate the genioglossus muscle to keep the airway open.This procedure shows a success rate that ranges from 72.4% to 75% at 12 months and 60 months, respectively. A number of technical difficulties and complications associated with this procedure include pleural effusion, pneumothorax, and lead migration into the pleural space. The procedure entails general anesthesia and is done on an outpatient basis. The recovery usually takes a few days.
- Hypopharyngeal surgery entails a wide variety of techniques that reposition, partially remove, shrink, or tighten the tongue muscle to treat the blockage of breathing in the lower part of the throat.The success rate for these procedures is variable, ranging from 23% to 83%, and some of them are often performed in conjunction with UPPP to maximize outcomes. The risks associated with hypopharyngeal surgeries include infection, dysphagia, haematoma, altered taste, injury to the genioglossus muscle, and paraesthesia of the lower teeth. Tongue surgeries are performed using general anesthesia and require a one-day stay in the hospital. Recovery typically takes up to 3 weeks.
- Soft-palate implant surgery is a minimally invasive procedure involving the insertion of a number of implants into the soft palate to stiffen it. This helps reduce vibration that causes symptoms of OSA.According to research published on NCBI, palatal implants are highly effective for reducing daytime sleepiness and improving snoring intensity in people with mild to moderate OSA symptoms, resulting in a higher quality of life. The risk of complications is low, with implant extrusion being the most prevalent problem. Soft-palate implant surgery is an office-based procedure that entails local anesthesia. Recovery takes only a few days.
- Nasal surgical procedures consist of septoplasty and turbinate reduction that straighten the nasal septum dividing your nostrils and shrink the enlarged turbinate tissue responsible for cleansing and humidifying the air entering your nose. These procedures can be performed together to make the airway bigger and minimize sleep-related symptoms.Nasal surgery is often pivotal in the entire surgical treatment of OSA and is critical for improving the patient's nasal breathing, reducing snoring, and increasing daily energy levels. Postoperative temporary bleeding and nasal congestions are the most prevalent complications for most intranasal procedures. More severe complications, such as a CSF fluid leak, are possible but unlikely. Nasal surgery is carried out under general anesthesia and takes about an hour. You can expect to return home the same day as surgery and recover fully in about a week.
In general, sleep apnea surgery options provide long-term benefits in appropriately selected patients. However, surgery does not completely eliminate OSA.
Even after proper surgical treatment from one of the leading sleep disorder doctors in NJ, persistent obstruction with associated symptoms may still be present in some patients. In practice, accomplishing treatment goals without patients' cooperation can be incredibly challenging, especially when it comes to weight loss and maintaining a healthy lifestyle.
Frequently Asked Questions
Sleep apnea is characterized by a pause in breathing during sleep, usually lasting between 10 seconds and up to a minute. Below are some frequently asked questions about this sleep condition.
What Is Sleep Apnea?
Sleep apnea is when your breathing stops and repeatedly starts during sleep. This may happen up to a hundred times throughout the night. It causes your brain to not get enough oxygen and your sleep to be disturbed.
What Are the Signs of Sleep Apnea?
Some warning sleep apnea symptoms include:
- Snoring;
- Daytime fatigue;
- Morning headaches;
- Choking sounds during sleep.
It is difficult to assess if you have sleep conditions on your own, but if you get a full night of sleep and still feel tired, that might be a warning sign. Your bed partner can also tell you if you snore, stop breathing at night, or gasp for air in your sleep.
What Causes Sleep Apnea?
Sleep apnea can be caused by certain lifestyle or genetic factors. Things like excessive weight or a thicker neck may cause it because these things usually cause constricted airways. Smoking, nasal congestion, or simply family history may also be causes of sleep apnoea.
What Are the Types of Sleep Apnea?
There are three types of sleep apnea: obstructive, central, and complex sleep apnoea.
Obstructive is when the muscles in the back of your throat relax. When these muscles relax, your airways close, preventing you from breathing.
Usually, your brain notices that you are not getting enough air and wakes you up so you can begin breathing. This awakening is usually very short, so you do not remember it.
Central sleep apnea is when your brain does not transmit the signal to your body to breathe. This means that you make no effort to breathe and your body soon wakes you up. This type of sleep disorder is less common.
Complex sleep apnea combines characteristics of both obstructive and central sleep apnea. Patients with this unique breathing pattern exhibit an upper airway obstruction as well as clinical features similar to respiratory control instability.
What Are Sleep Apnea Side Effects?
The most common side effect of sleep apnea is not feeling well when you wake up. People are usually tired throughout the day, even if they got enough sleep.
You may also experience headaches and a sore throat in the morning. If you are suffering from this condition, you usually wake up throughout the night, although for short enough periods that you do not remember, leaving you feeling tired in the morning.
What Are the Risk Factors for OSA?
Various sleep apnea risk factors have already been identified. But the most dramatic risk factor is obesity, which is reflected by multiple criteria, including BMI, waist-to-hip ratio, and neck circumference. Dr. Tadros differentiates between two groups of risk factors:
Modifiable risk factors for OSA
- Obesity
- Smoking (both active and passive)
- Supine body position during sleep
- Drugs (alcohol and opiates intake)
- Nasal obstruction or congestion
Non-modifiable risk factors for OSA
- Aging (up to the age of 65)
- Male gender
- Race
- Menopause
- Genetic predisposition
- Craniofacial anatomy
How to Test for Sleep Apnea
If you are suffering from sleep apnea in NYC & NJ, Dr. Monica Tadros uses a nocturnal polysomnography test to confirm the diagnosis. For this test, you are hooked up to a machine while you sleep that tests your heart rate, lung and brain activity, movement, and breathing patterns.
Your insurance should cover this test. Sometimes your doctor can provide you with a home test that will measure your breathing levels and oxygen levels during your sleep.
What Is the Epidemiology of Obstructive Sleep Apnea?
According to NCBI, approximately 2% of women and 4% of men suffer from OSA in the United States. More recently, prevalence is higher in African American, Hispanic and Asian populations.
It has also been confirmed that susceptibility to this condition increases with age when individuals reach the age of 50 or more.
Can You Die From Sleep Apnea?
Sleep apnea is linked to other fatal diseases like heart disease and high blood pressure. It can increase your risk of sudden cardiac death. If you have sleep apnea, you are also more likely to have a stroke, diabetes, and depression.
Request your sleep apnea treatment consultation today with Dr. Monica Tadros at her center for facial plastic surgery. Please use the contact form to receive additional information or call NYC: (201) 408-5430 or NJ: (201) 408-5430.