Two terms you’ve heard paired with COVID-19 are respirator and ventilator. While we’ve heard the terms in similar context, they serve two very different, while important, purposes. So, what’s the difference between a respirator and a ventilator?
The short answer is that respirators are worn by front-line healthcare professionals for protection against infection, while ventilators are used by patients fighting respiratory illnesses to get the oxygen they need to survive. Let’s dive deeper into the respiratory system and its role when it comes to COVID-19.
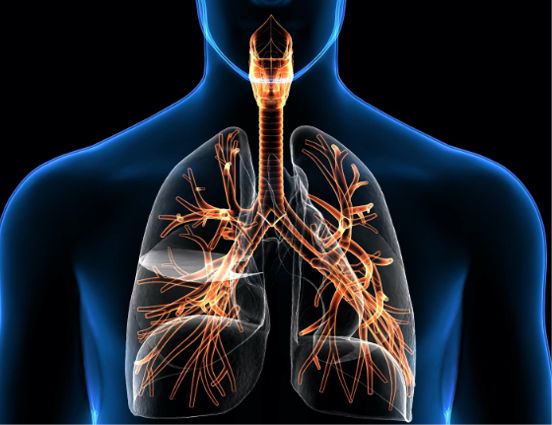
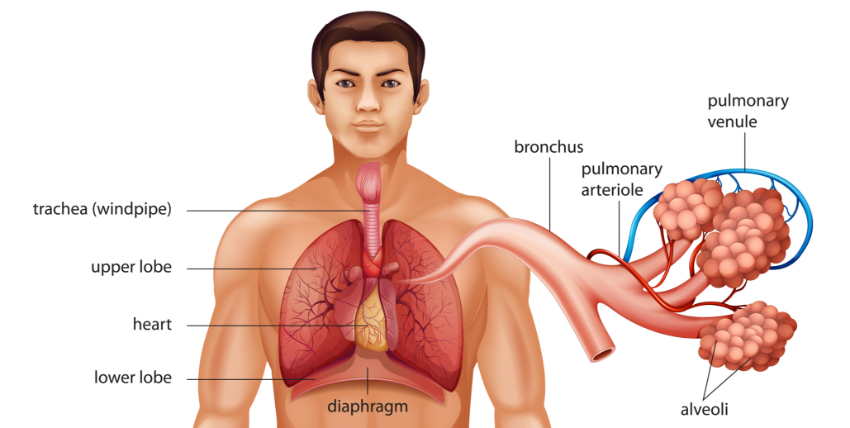
The respiratory and cardiovascular systems of the human body are intricately connected to serve a specific life-sustaining purpose: collecting and distributing oxygen throughout the body, while expelling unwanted carbon dioxide. Without a constant supply of oxygen, a condition called hypoxia, cells die of strangulation. Similarly, if carbon dioxide builds up within the tissues, cells malfunction and die. Both conditions can lead to organ failure and even death. The airways of the respiratory system:
- Move oxygen to the lungs and carbon dioxide out
- Control the temperature and moisture content of those gases
- Are the first line of defense against harmful matter trying to invade the body 1
The novel coronavirus (COVID-19) compromises these systems by reducing oxygen input to dangerous levels, leading to a condition known as acute respiratory distress syndrome (ARDS). Once ARDS develops, the recommended treatment involves connecting the patient to a ventilator. The ventilator takes over for the respiratory system to move oxygen through the lungs to the rest of the body.2
Until now, most respiratory illnesses resulted from serious conditions such as alcoholism, pneumonia and sepsis. Any respiratory ailment is often a sign of a fast-moving disease. Lung problems can be life-threatening and usually require immediate treatment.
Treatment for respiratory illnesses has proven successful for many years, although many patients suffer long-term respiratory consequences, such a chronic lung disease and fatigue. There is much that’s yet unknown about the COVID-19 disease, however. For example, no one’s sure how it’s primarily contracted or what long-term effects it will have on the body following ventilation. That’s why prevention still remains the primary focus of efforts to stop the coronavirus.
Ventilators for Breathing Treatment
Although the terms often have been used interchangeably, there is actually a distinct difference between a respirator and a ventilator. Respirators are used for prevention, while ventilators are used for treatment. 3 Basically, ventilators do the breathing for people who have lost the ability to breathe on their own. Ventilators send oxygen into the patients’ airways through a breathing tube. The tube is inserted through the mouth or the nose to reach the throat.
Since this can be an uncomfortable procedure, the patient may receive some type of anesthesia while a health care worker inserts the tube. The tube is attached to a holder that directs the tube over the head. It may be taped to the face to keep it out of the way.
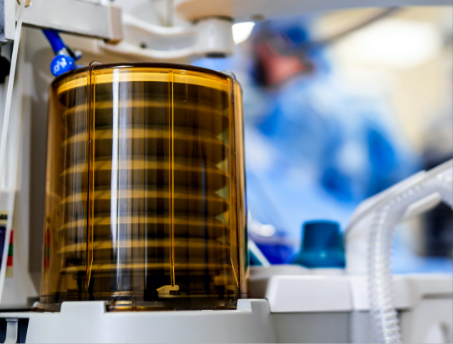
The breathing tube also may be inserted through a hole in the throat in a procedure called a tracheostomy.7 Since the tube passes through the vocal cords, the patient is unable to speak. Eating also is impossible, so a feeding tube provides nutrients intravenously.
Blood tests and chest x-rays are employed periodically to check oxygen levels while a ventilator is in place. A computer attached to the ventilator allows medical personnel to make adjustments as needed. The breathing tube also must be suctioned regularly to prevent mucus from accumulating. Ventilators also come with various other risks, including:
- An infection that leads to pneumonia, called ventilator-associated pneumonia (VAP). Sinus infections also may occur. Both conditions may respond to antibiotics.
- Pneumothorax, or when air leaks from the lungs into the space between the chest wall and the lungs. This medical condition may be fatal, as it can lead to collapsed lungs.
- Lung damage caused by high levels of oxygen or excessive pressure from the rush of oxygen.
- Vocal cord damage. The breathing tube can irritate or damage the nerves of the vocal cords, causing vocal cord paralysis, a serious condition.
Although the terms often have been used interchangeably, there is actually a distinct difference between a respirator and a ventilator. Respirators are used for prevention, while ventilators are used for treatment.
As the patient recovers and gains strength, the medical team attempts to wean the person off the ventilator. This occurs slowly at first, usually while the vent is still in place. Once breathing resumes normally, the breathing tube is removed. 5 and 6
Respirators and Face Masks
Respirators should be reserved for critical care providers. Most people, such as those who don’t work directly with patients infected with COVID-19, don’t need to wear these protective masks. Unless you suspect you’re going to be in close contact with a carrier of the virus, an appropriately thick face mask is sufficient to prevent the spread of the disease. Not touching your face and washing your hands frequently are other effective preventative measures.
There is a major difference between face masks and respirators:
• Surgical masks and face masks are produced commercially primarily to protect the wearer from expelling virulent particles transmitted by mucus and spit while sneezing or coughing. Most people are using face masks as part of their COVID-19 prevention strategy. The masks are designed to trap the particles in the mask, which is why it’s important to wash a cloth, reusable mask after wearing it.
• Respirators, on the other hand, provide a filtration system to remove harmful particulate that the wearer breathes in. When properly fitted, respirators prevent up to 95 percent of the contagious particles from reaching the wearer’s respiratory system — hence the name “N95.” These protective masks usually are reserved for single use, but because of the national shortage, some measures have been taken to sanitize them for reuse.
The Centers for Disease Control and Prevention (CDC) recommends that when individuals are working in areas where the exposure to the virus is especially high, they should don respirators, such as the popular N95 kind. It’s vital that a respirator, when worn, provides a tight seal around the face. Beards and other facial hair may prevent the necessary seal and compromise the integrity of the protection. 4
- References:
- Ref 1: Marion Richardson, BD, CertEd, RGN, RNT, DipN, is senior lecturer/programme leader, emergency nursing, Department of Nursing and Midwifery, University of Hertfordshire [See source 1]
- Ref 2: National Heart, Lung and Blood Institute [See source 5]
- Sources:
- 1. https://www.nursingtimes.net/clinical-archive/respiratory-clinical-archive/the-respiratory-system-part-1-nose-pharynx-and-larynx-23-05-2006/
- 2. https://health.clevelandclinic.org/heres-the-damage-coronavirus-covid-19-can-do-to-your-lungs/
- 3. https://www.govtech.com/em/emergency-blogs/disaster-zone/what-is-the-difference-between-a-ventilator-and-a-respirator.html
- 4. https://multimedia.3m.com/mws/media/956213O/differences-between-respirators-and-masks.pdf?fn=Respirator%20vs%20Surgical%20Mask%20flye
- 5. https://www.nhlbi.nih.gov/health-topics/ventilatorventilator-support
- 6. https://medlineplus.gov/ency/patientinstructions/000458.htm
- 7. https://www.mayoclinic.org/tests-procedures/tracheostomy/about/pac-20384673